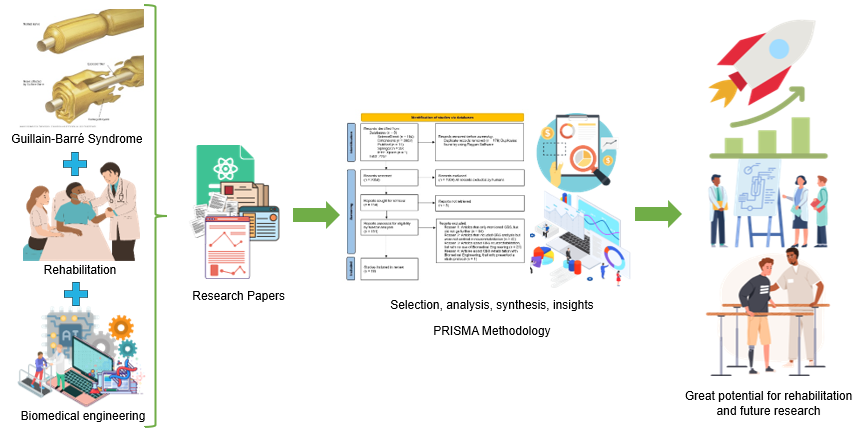
Use of Biomedical Engineering for Rehabilitation of Patients with Disability Caused by Guillain-Barré Syndrome: a Systematic Review
DOI:
https://doi.org/10.17488/RMIB.45.1.4Keywords:
Biomedical engineering, Guillain-Barré Syndrome, neurorehabilitation, rehabilitation deviceAbstract
This systematic review aims to assess the extent to which biomedical engineering has been applied in the rehabilitation of patients suffering from Guillain-Barré Syndrome (GBS), given the scarcity of information on this topic. We conducted a thorough analysis of research articles, conference abstracts, and case reports published between 2000 and 2023, specifically from ScienceDirect, PubMed, IEEE Xplore, Springer, and Dimensions. 19 articles were extensively discussed, complemented by an additional 40 information sources providing supplementary information. Each paper underwent a meticulous review process by the four authors, where each separately examined the title and abstract of the papers and subsequently provided a thorough examination of the full text; when conflicts arose, a clear consensus was reached through discussion. The analysis of the articles revealed a notable improvement in upper and lower limb function of GBS patients that was facilitated by both custom-made and commercial devices. Likewise, a small handful of other devices have been used (e.g., to improve urinary retention issues). There is a clear opportunity for new research, innovation and applications.
Downloads
References
B. van den Berg, C. Walgaard, J. Drenthen, C. Fokke, B. C. Jacobs, and P. A. Van Doorn, “Guillain-Barré syndrome: Pathogenesis, diagnosis, treatment and prognosis,” Nat. Rev. Neurol., vol. 10, no. 8, pp. 469-482, 2014, doi: https://doi.org/10.1038/nrneurol.2014.121
H. J. Willison, B. C. Jacobs, and P. A. van Doorn, “Guillain- Barré syndrome,” Lancet, vol. 388, no. 10045, pp. 717–727, Aug. 2016, doi: https://doi.org/10.1016/s0140-6736(16)00339-1
A. Créange, “Guillain-Barré syndrome: 100 years on,” Rev. Neurol., vol. 172, no. 12, pp. 770-774, Dec. 2016, doi: https://doi.org/10.1016/j.neurol.2016.10.011
N. Shahrizaila, H. C. Lehmann, and S. Kuwabara, “Guillain-Barré syndrome,” Lancet, vol. 397, no. 10280, pp. 1214–1228, Mar. 2021, doi: https://doi.org/10.1016/s0140-6736(21)00517-1
A. Mirian, M. W. Nicolle, and A. Budhram, “Guillain– Barré syndrome,” Can. Med. Assoc. J., vol. 193, no. 11, pp. E378–E378, Mar. 2021, doi: https://doi.org/10.1503/cmaj.202710
J. Expósito, L. Carrera, D. Natera, G. Nolasco, A. Nascimento, and C. Ortez, “Síndrome de Guillain-Barré y otras neuropatías autoinmunes: tratamiento actual,” Med., vol. 82, no. 3, pp. 82–88, 2022. [Online]. Available: https://www.medicinabuenosaires.com/revistas/vol82-22/s3/82s3.pdf
M. M. Dimachkie and R. J. Barohn, “Guillain-Barré Syndrome and Variants,” Neurol. Clin., vol. 31, no. 2, pp. 491–510, May 2013, doi: https://doi.org/10.1016/j.ncl.2013.01.005
S. R. Sudulagunta, M. B. Sodalagunta, M. Sepehrar, H. Khorram, et al., “Guillain-Barré syndrome: clinical profile and management,” Ger. Med. Sci., vol. 13, art. no. Doc16, Sep. 2015, doi: https://doi.org/10.3205/000220
M. R. Ashrafi, A. Mohammadalipoor, A. R. Naeini, M. Amanat, et al., “Clinical Characteristics and Electrodiagnostic Features of Guillain-Barré Syndrome Among the Pediatric Population,” J. Child. Neurol., vol. 35, no. 7, pp. 448–455, Jun. 2020, doi: https://doi.org/10.1177/0883073820905157
T. Harbo and H. Andersen, “Neuromuscular effects and rehabilitation in Guillain-Barré syndrome,” in Zika Virus Impact, Diagnosis, Control, and Models, C. R. Martin, V. R. Preedy, C. J. Hollins Martin, R. Rafendram, Eds., Oxford, United Kingdom: Elsevier, 2021, ch. 2, pp. 143– 149, doi: https://doi.org/10.1016/B978-0-12-820267-8.00013-3
F. Khan and B. Amatya, “Rehabilitation interventions in patients with acute demyelinating inflammatory polyneuropathy: a systematic review,” Eur. J. Phys. Rehabil. Med., vol. 48, no. 3, pp. 507–522, Sep. 2012. [Online]. Available: https://www.minervamedica.it/en/journals/europa-medicophysica/article.php?cod=R33Y2012N03A0507
P. A. van Doorn, L. Ruts, and B. C. Jacobs, “Clinical features, pathogenesis, and treatment of Guillain-Barré syndrome,” Lancet Neurol., vol. 7, no. 10, pp. 939–950, Oct. 2008, doi: https://doi.org/10.1016/s1474-4422(08)70215-1
B. R. Wakerley and N. Yuki, “Pharyngeal-cervical-brachial variant of Guillain-Barre syndrome,” J. Neurol. Neurosurg. Psychiatry, vol. 85, no. 3, pp. 339–344, Mar.
, doi: https://doi.org/10.1136/jnnp-2013-305397
B. S. Schoenberg, “Epidemiology of Guillain-Barré syndrome,” Adv. Neurol., vol. 19, pp. 249–60, 1978.
N. S. Arsenault, P.-O. Vincent, Y. B. H. Shen, R. Bastien, A. Sweeney, “Influence of exercise on patients with Guillain-Barré syndrome: A systematic review,” Physiother. Can., vol. 68, no. 4, pp. 367–376, 2016, doi: https://doi.org/10.3138/ptc.2015-58
J. B. Bussmann, M. P. Garssen, P. A. van Doom, and H. J. Stam, “Analysing the favourable effects of physical exercise: Relationships between physical fitness, fatigue and functioning in Guillain-Barré syndrome and chronic inflammatory demyelinating polyneuropathy,” J. Rehabil. Med., vol. 39, no. 2, pp. 121–125, Mar. 2007, doi: https://doi.org/10.2340/16501977-0007
S. Jones, W. D. Man, W. Gao, I. J. Higginson, A. Wilcock, and M. Maddocks, “Neuromuscular electrical stimulation for muscle weakness in adults with advanced disease,” Cochrane Database of Syst. Rev., vol. 2016, no. 10, art. no. CD009419, Oct. 2016, doi: https://doi.org/10.1002/14651858.cd009419.pub3
M. J. Page, D. Moher, P. M. Bossuyt, I. Boutron, et al., “PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews,” BMJ, vol. 372, art. no. n160, Mar. 2021, doi: https://doi.org/10.1136/bmj.n160
L. M. Kmet, R. C. Lee, and L. S. Cook, Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields. Alberta Heritage Foundation for Medical Research, 2004, doi: https://doi.org/10.7939/R37M04F16
S. Albiol-Pérez, M. Forcano-García, M. T. Muñoz-Tomás, P. Manzano-Fernández, S. Solsona-Hernández, M. A. Mashat, J. A. Gil-Gómezet, “A novel virtual motor rehabilitation system for guillain-barré syndrome: Two single case studies,” Methods Inf. Med., vol. 54, no. 2, pp. 127–134, 2015, doi: https://doi.org/10.3414/me14-02-0002
Y. Fang and Z. F. Lerner, “Bilateral vs. Paretic-Limb-Only Ankle Exoskeleton Assistance for Improving Hemiparetic Gait: A Case Series,” IEEE Robot Autom. Lett., vol. 7, no. 2, pp. 1246–1253, Apr. 2022, doi: https://doi.org/10.1109/lra.2021.3139540
S. Tanida, T. Kikuchi, T. Kakehashi, K. Otsuki, et al., “Intelligently controllable Ankle Foot Orthosis (I- AFO) and its application for a patient of Guillain-Barre syndrome,” in 009 IEEE International Conference on Rehabilitation Robotics, Kyoto, Japan, 2009, pp. 857-862, doi: https://doi.org/10.1109/ICORR.2009.5209590
N. Jamshidi, M. Rostami, S. Najarian, M. B. Menhaj, M. Saadatnia, and S. Firooz, “Modelling of human walking to optimise the function of ankle-foot orthosis in Guillan- Barré patients with drop foot,” Singapore Med. J., vol. 50, no. 4, pp. 412-417, Apr. 2009. [Online]. Available: http://smj.sma.org.sg/5004/5004a13.pdf
F. Chrif, H. J. A. van Hedel, M. Vivian, T. Nef, and K. J. Hunt, “Usability evaluation of an interactive leg press training robot for children with neuromuscular impairments,” Technol. Health Care, vol. 30, no. 5, pp. 1183– 1197, Mar. 2022, doi: https://doi.org/10.3233%2FTHC-213629
K.-S. Lee, J.-H. Park, J. Beom, and H.-S. Park, “Design and evaluation of passive shoulder joint tracking module for upper-limb rehabilitation robots,” Front. Neurorobot., vol. 12, art. no. 38, Jul. 2018, doi: https://doi.org/10.3389/fnbot.2018.00038
A. Meyer-Heim, I. Borggraefe, C. Ammann-Reiffer, St. Berweck, et al., “Feasibility of robotic-assisted locomotor training in children with central gait impairment,” Dev. Med. Child Neurol., vol. 49, no. 12, pp. 900–906, Dec. 2007, doi: https://doi.org/10.1111/j.1469-8749.2007.00900.x
J. Tuckey and Greenwood R., “Rehabilitation after severe Guillain–Barré syndrome - the use of partial body weight support,” Physiother. Res. Int., vol. 9, no. 2, pp. 96–103, 2004, doi: https://doi.org/10.1002/pri.306
M. Bolliger, R. Banz, V. Dietz, and L. Lünenburger, “Standardized voluntary force measurement in a lower extremity rehabilitation robot,” J. Neuroeng. Rehabil., vol. 5, art. no. 5, Oct. 2008, doi: https://doi.org/10.1186/1743-0003-5-23
D. Wille, K. Eng, L. Holper, E. Chevrier, et al., “Virtual reality-based paediatric interactive therapy system (PITS) for improvement of arm and hand function in children with motor impairment a pilot study,” Dev. Neurorehabil., vol. 12, no. 1, pp. 44–52, Feb. 2009, doi: https://doi.org/10.1080/17518420902773117
P. Bulley, “The podiatron: an adjunct to physiotherapy treatment for Guillain–Barré syndrome?,” Physiother. Res. Int., vol. 8, no. 4, pp. 210–215, Nov. 2003, doi: https://doi.org/10.1002/pri.291
M. S. Wosnitzer, R. Walsh, and M. P. Rutman, “The use of sacral neuromodulation for the treatment of non- obstructive urinary retention secondary to Guillain-Barré syndrome” Int. Urogynecol. J. Pelvic Floor Dysfunct., vol. 20, no. 9, pp. 1145– 1147, Sep. 2009, doi: https://doi.org/10.1007/s00192-009-0826-9
K. Laver, F. Lim, K. Reynolds, S. George, J. Ratcliffe, S. Sim, M. Crotty, “Virtual Reality Grocery Shopping Simulator: Development and Usability in Neurological Rehabilitation,” Presence, vol. 21, no. 1, pp. 183–191,
Feb. 2012, doi: https://doi.org/10.1162/PRES_a_00098
S. Choi, S. W. Kim, H. R. Jeon, J. S. Lee, D. Y. Kim, and J. W. Lee, “Feasibility of Robot-Assisted Gait Training with an End-Effector Type Device for Various Neurologic Disorders” Brain Neurorehabil., vol. 13, no. 1, art. no. e6, Nov. 2019, doi: https://doi.org/10.12786/bn.2020.13.e6
S. Y. Rhee, H. Jeon, S. W. Kim, and J. S. Lee, “The effect of an end-effector type of robot-assisted gait training on patients with Guillain-Barre syndrome: a cross-sectional study,” F1000Res, vol. 9, art. no. 1465, 2020, doi: https://doi.org/10.12688/f1000research.26246.1
L. Kauhanen, P. Jylänki, J. Lehtonen, P. Rantanen, H. Alaranta, and M. Sams, “EEG-based brain-computer interface for tetraplegics,” Comput. Intell. Neurosci., vol. 2007, art. no. 23864, 2007, doi: https://doi.org/10.1155%2F2007%2F23864
Y. Takahashi, T. Terada, K. Inoue, Y. Ito, Y. Ikeda, H. Lee, T. Komeda, “Haptic Device System for Upper Limb Motor and Cognitive Function Rehabilitation: Grip Movement Comparison between Normal Subjects and Stroke Patients” in 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, Netherlands, 2007, pp. 736-741, doi: https://doi.org/10.1109/ICORR.2007.4428507
A. Nehrujee, H. Andrew, Reethajanetsurekha, A. Patricia, et al., “Plug-and-train robot (pluto) for hand rehabilitation: Design and preliminary evaluation,” IEEE Access, vol. 9, pp. 134957–134971, 2021, doi: https://doi.org/10.1109/ACCESS.2021.3115580
N. Céspedes, M. Múnera, C. Gómez, and C. A. Cifuentes, “Social Human-Robot Interaction for Gait Rehabilitation,” IEEE Trans. Neural Syst. Rehabil. Eng., vol. 28, no. 6, pp. 1299–1307, Jun. 2020, doi: https://doi.org/10.1109/TNSRE.2020.2987428
Clarivate. “Journal Citation Reports.” Clarivate. https://clarivate.com/products/scientific-and-academic-research/research-analytics-evaluation-and-management-solutions/journal-citation-reports/ (accessed 2023).
J. J. Sejvar, A. L. Baughman, M. Wise, and O. W. Morgan, “Population incidence of Guillain-Barré syndrome: A systematic review and meta-analysis,” Neuroepidemiology, vol. 36, no. 2. pp. 123–133, Apr. 2011, doi: https://doi.org/10.1159/000324710
United Nations, “World Economic Situation and Prospects 2022,” United Nations. 2022. Accessed: May 23, 2023. [Online]. Available: https://www.un.org/development/desa/dpad/publication/world-economic-situation-and-prospects-2022/
United Nations, “World Population Prospects 2022: Summary of Results,” New York, 2022. United Nations. 2022. Accessed: 2023. [Online]. Available: https://www.un.org/development/desa/pd/content/World-Population-Prospects-2022
D. S. M. Ong, M. Z. Weibin, and R. Vallabhajosyula, “Serious games as rehabilitation tools in neurological conditions: A comprehensive review,” Technol.Health Care, vol. 29, no. 1, pp. 15–31, Jan. 2021, doi: https://doi.org/10.3233/thc-202333
A. Jackson, C. T. Carnel, J. F. Ditunno, M. S. Read, et al., “Outcome Measures for Gait and Ambulation in the Spinal Cord Injury Population,” J. Spinal Cord. Med., vol. 31, no. 5, pp. 487–499, Jan. 2008, doi: https://doi.org/10.1080/10790268.2008.11753644
O. Beauchet, B. Fantino, G. Allali, S. W. Muir, M. Montero- Odasso, and C. Annweiler, “Timed up and go test and risk of falls in older adults: A systematic review,” J. Nutr. Health Aging., vol. 15, no. 10, pp. 933–938, Dec. 2011, doi: https://doi.org/10.1007/s12603-011-0062-0
E. Barry, R. Galvin, C. Keogh, F. Horgan, and T. Fahey, “Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta- analysis,” BMC Geriatr., vol. 14, no. 1, art. no. 14, Dec. 2014, doi: https://doi.org/10.1186/1471-2318-14-14
R. P. Kleyweg, F. G. A. van der Meché, and P. I. Schmitz, “Interobserver agreement in the assessment of muscle strength and functional abilities in Guillain-Barré syndrome,” Muscle Nerve, vol. 14, no. 11, pp. 1103–1109, Nov. 1991, doi: https://doi.org/10.1002/mus.880141111
G. Scivoletto, F. Tamburella, L. Laurenza, C. Foti, J. F. Ditunno, and M. Molinari, “Validity and reliability of the 10-m walk test and the 6-min walk test in spinal cord injury patients,” Spinal Cord., vol. 49, no. 6, pp. 736–740, Jun. 2011, doi: https://doi.org/10.1038/sc.2010.180
H. J. A. van Hedel, M. Wirz, and V. Dietz, “Standardized assessment of walking capacity after spinal cord injury: the European network approach,” Neurol. Res., vol. 30, no. 1, pp. 61–73, Feb. 2008, doi: https://doi.org/10.1179/016164107x230775
K. Bennell, F. Dobson, and R. Hinman, “Measures of physical performance assessments: Self-Paced Walk Test (SPWT), Stair Climb Test (SCT), Six-Minute Walk Test (6MWT), Chair Stand Test (CST), Timed Up & Go (TUG), Sock Test, Lift and Carry Test (LCT), and Car Task,” Arthritis Care Res. (Hoboken), vol. 63, no. S11, pp. S350–S370, Nov. 2011, doi: https://doi.org/10.1002/acr.20538
S. T. Larson and J. Wilbur, “Muscle Weakness in Adults: Evaluation and Differential Diagnosis,” Am. Fam. Physician, vol. 101, no. 2, pp. 95–108, Jan. 2020. [Online]. Available: https://www.aafp.org/pubs/afp/issues/2020/0115/p95.html
T. Paternostro-Sluga, M. Grim-Stieger, M. Posch, O. Schuhfried, et al., “Reliability and validity of the Medical Research Council (MRC) scale and a modified scale for testing muscle strength in patients with radial palsy,” J. Rehabil. Med., vol. 40, no. 8, pp. 665–671, Aug. 2008, doi: https://doi.org/10.2340/16501977-0235
N. Maclean and P. Pound, “A critical review of the concept of patient motivation in the literature on physical rehabilitation,” Soc. Sci. Med., vol. 50, no. 4, pp. 495–506, Feb. 2000, doi: https://doi.org/10.1016/s0277-9536(99)00334-2
A. Kusec, D. Velikonja, C. DeMatteo, and J. E. Harris, “Motivation in rehabilitation and acquired brain injury: can theory help us understand it?,” Disabil. Rehabil., vol. 41, no. 19, pp. 2343–2349, Sep. 2019, doi: https://doi.org/10.1080/09638288.2018.1467504
P. Meyns, T. Roman de Mettelinge, J. van der Spank, M. Coussens, and H. Van Waelvelde, “Motivation in pediatric motor rehabilitation: A systematic search of the literature using the self-determination theory as a conceptual framework,” Dev. Neurorehabil., vol. 21, no. 6, pp. 371-390, Aug. 2018, doi: https://doi.org/10.1080/17518423.2017.1295286
Y. Nishiwaki, M. Nakamura, and M. Nihei, “A novel method of evaluating changes in intrinsic motivation during cognitive rehabilitation,” in 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Mexico, 2021, pp. 2095-2099, doi: https://doi.org/10.1109/EMBC46164.2021.9630738
G. Verrienti, C. Raccagni, G. Lombardozzi, D. De Bartolo, and M. Iosa, “Motivation as a Measurable Outcome in Stroke Rehabilitation: A Systematic Review of the Literature,” Int. J. Environ. Res. Public Health, vol. 20, no. 5, art. no. 4187, Feb. 2023, doi: https://doi.org/10.3390/ijerph20054187
Z. Zhou, J. Li, H. Wang, Z. Luan, Y. Li, and X. Peng, “Upper limb rehabilitation system based on virtual reality for breast cancer patients: Development and usability study,” PLoS One, vol. 16, no. 12, art. no. e0261220, Dec. 2021, doi: https://doi.org/10.1371/journal.pone.0261220
E. L. Friesen, “Measuring AT Usability with the Modified System Usability Scale (SUS),” Stud. Health Technol. Inform., vol. 242, pp. 137–143, 2017. [Online]. Available: https://ebooks.iospress.nl/publication/47262
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Revista Mexicana de Ingenieria Biomedica

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Upon acceptance of an article in the RMIB, corresponding authors will be asked to fulfill and sign the copyright and the journal publishing agreement, which will allow the RMIB authorization to publish this document in any media without limitations and without any cost. Authors may reuse parts of the paper in other documents and reproduce part or all of it for their personal use as long as a bibliographic reference is made to the RMIB. However written permission of the Publisher is required for resale or distribution outside the corresponding author institution and for all other derivative works, including compilations and translations.